42
Home Delivery from Amazon Pharmacy
A new way to save on medications
Amazon Pharmacy oers a home delivery service that lets you easily order and quickly get your non-specialty prescription
medication
1
delivered at home.
And as a Florida Blue member, you get access to MedsYourWay
™
prescription drug discount card pricing. The prescription
discount card
2
gives you up to 80% savings
3
on brand and generic medicines and is seamlessly built into the Amazon Pharmacy
experience. You can get the lowest cost available while saving time and money. Using the MedsYourWay discount card is not
insurance; however, using it for covered medications
4
will also count toward your out-of-pocket maximum.
SHOPSHOP
Easy to use
Amazon Pharmacy makes ordering your medications easier because it’s like shopping on Amazon:
• Easy sign up, which includes the option to have your account auto-populated with your
prescription history.
• Option for 90
+
day supply.
• Pharmacists on call 24/7.
• Ability to manage your medication and order history.
SAVESA VE
Built-in drug discount card
Some drugs may be available at lower prices with a discount card. MedsYourWay discount pricing
is built right into the Amazon Pharmacy experience.
• At check out, you’ll see the lowest cost available for your medication. That’s the price you’ll pay.
• MedsYourWay discount card pricing is not insurance; however, all prescribed and covered
purchases, whether paying a copay or using the discount card pricing, automatically count
toward your annual out-of-pocket maximum.
SHIPSHIP
Convenient home delivery
Skip the pharmacy line with home delivery.
• Fast delivery: Amazon Prime members get 2-day no-cost shipping on most orders; standard
no-cost shipping for non-Amazon Prime members is 5-day but can be expedited to 2-day
delivery for an additional fee.
• Real-time package tracking from order to delivery.
To learn more about Amazon Pharmacyʼs home delivery services, call the number on the back of your member ID card and
say, “Pharmacy.”
Or log on to your Florida Blue Member Account and see the Pharmacy section under My Plan.
1 Amazon Pharmacy does not dispense Schedule 2 controlled substance drugs.
2 MedsYourWay prescription drug discount card, administered by Inside Rx LLC, is not insurance. You are responsible for the cost of prescription(s) when using the card. Limitations apply.
The discount pricing card is automatically available to all members with no additional sign up needed. The card is electronic only, a physical card will not be mailed.
3 Average savings based on usage and Inside Rx data as compared to cash prices; average savings are up to 80% for all generics and 37% for select brand medicines. Restrictions apply.
4 If your medicine has an unfullled requirement, the cost may not count towards your (accumulator) out-of-pocket maximum. Typical requirements include prior authorization (PA) needed,
quantity limit exceeded or step therapy needed.
Amazon Pharmacy is an independent company contracted to provide Pharmacy Home Delivery services for both Florida Blue and Florida Blue HMO. Health insurance is oered by Florida Blue.
HMO coverage is oered by Florida Blue HMO, an aliate of Florida Blue. These companies are Independent Licensees of the Blue Cross Blue Shield Association. 109130 0322
7149-F1 FL 03/22 © 2021 Prime Therapeutics LLC 10014866
43
88785 0417
1
Walgreens can save you money
You’ll pay a lower price for many prescriptions at
Walgreens. Sometimes the savings will be big!
This means you’ll often pay less when you have a
deductible to meet. Or if the drug costs less than your
copay, you’ll pay the lower price
1
.
At the corner or online—you’ll find a
Walgreens near you
With more than 800 locations in Florida (many with
health care clinics) you’ll find a Walgreens close to
you. Add Walgreens’ mobile app to your smartphone,
and you can refill or transfer prescriptions, make a
personal shopping list, order photos and browse
weekly specials.
Moving your prescriptions
If you’re using a retail pharmacy other than Walgreens,
think about moving your prescriptions to Walgreens
today. You can view a list of Walgreens pharmacies at
floridablue.com/FxclusiveQharmacy
.
Here’s how to easily make the switch:
• Call or stop by your local Walgreens and tell the
pharmacist you want to move your prescriptions from
another pharmacy. They’ll help you make the switch.
Just have a list of your current medications handy.
• Using the free Walgreens mobile app on your
smartphone, take a picture of your medicine bottle
and send it to your nearest Walgreens.
If you continue to use a retail pharmacy other than
Walgreens in the new benefit year, you’ll experience
higher out-of-pocket costs.
• You’ll pay the full price of your medication out
of your pocket if you don’t have out-of-network
pharmacy benefits.
• If you have out-of-network pharmacy benefits, you’ll
pay the full price of your medication and can file a
claim for reimbursement. Your reimbursement will
be based on out-of-network benefits.
Please refer to your summary of benefits to see if you
have out-of-network pharmacy benefits. For greatest
savings and convenience, always use an in-network
pharmacy. If you currently fill prescriptions at a
Walgreens pharmacy, you don’t need to take any action.
Savings are
ComingYour
Way!
Your pharmacy network
is designed to save you
money. In the new benefit
year, Walgreens will be your
exclusive retail pharmacy.

Pasco County Schools: Pharmacy Benefit
44
Pharmacy Benefit
Provider: Prime Therapeutics, Florida Blue’s Pharmacy Benefit Manager
EFFECTIVE JANUARY 1, 2023 AMAZON PHARMACY
WILL BE THE NEW MAIL ORDER PROVIDER.
• NEW! Mail-order for up to a 90-day supply will be provided
through Amazon Pharmacy, where you’ll have access to
MedsYourWay
TM
discount card pricing. You pay less for ordering a
90-day supply by mail, rather than going to a retail pharmacy, one
month at a time.
• Effective January 1, 2023, Walgreens will continue to be your
exclusive retail pharmacy. You may only fill prescriptions for
non-specialty generic and Brand Name drugs at your local
Walgreens retail pharmacy. Using any other retail pharmacy
would be out of network for HMO members and NOT covered.
For PPO members, it would cost you more out of pocket and
you would have to pay upfront and file a claim for reimbursement.
• You have 2 options at Walgreens; up to a 30 day supply or up
to a 90-day supply for long-term medications.
• Fill your Self-Administered Specialty medications using
Accredo (1-888-425-5970). Some exceptions may apply for
certain Limited Distributed Drugs that cannot be filled by Accredo.
• Advise your doctor to fill all of your Provider-Administered
Specialty medications (Medical Pharmacy Benefit) using CVS
CareMark Specialty Pharmacy (1-866-278-5108) with the
exception of certain limited distribution drugs. Note: This does
not apply if your doctor subscribes to the Provider Administered
Drug Program (PADP).
The Drug Categories are:
• Generics:
These contain the same active ingredients as their brand name
equivalents, and offer the same effectiveness and safety.
They have the lowest copay.
• Preferred Brands:
These are brand name drugs that are preferred by the plan and
have a higher co-pay than their generic counterparts.
• Non-Preferred Brands:
These are higher cost because there is usually a generic or a
preferred brand drug available instead.
•
Specialty Drugs:
These are prescription medications that require special handling,
administration or monitoring. These medications are used to treat
chronic diseases or genetic disorders such as Multiple Sclerosis,
Rheumatoid Arthritis, Hepatitis C, and Hemophilia.
Prior Authorization Programs
(Responsible Steps and Responsible Quantity):
• Encourages the appropriate, safe and cost-effective use of
medication. If you are currently taking or are prescribed a
medication that is included in the Prior Authorization Program,
your physician will need to submit a request form in order for your
prescription to be considered for coverage. If you do not request
and/or receive prio approval, the medication will not be covered.
A current listing of drugs requiring prior authorization are
indicated in the prior authorization column following the product
name in the Medication Guide which can be found online at
www.floridablue.com.
Florida Blue 800.507.9820 or visit www.floridablue.com
Pasco County Schools: Pharmacy Benefit
45
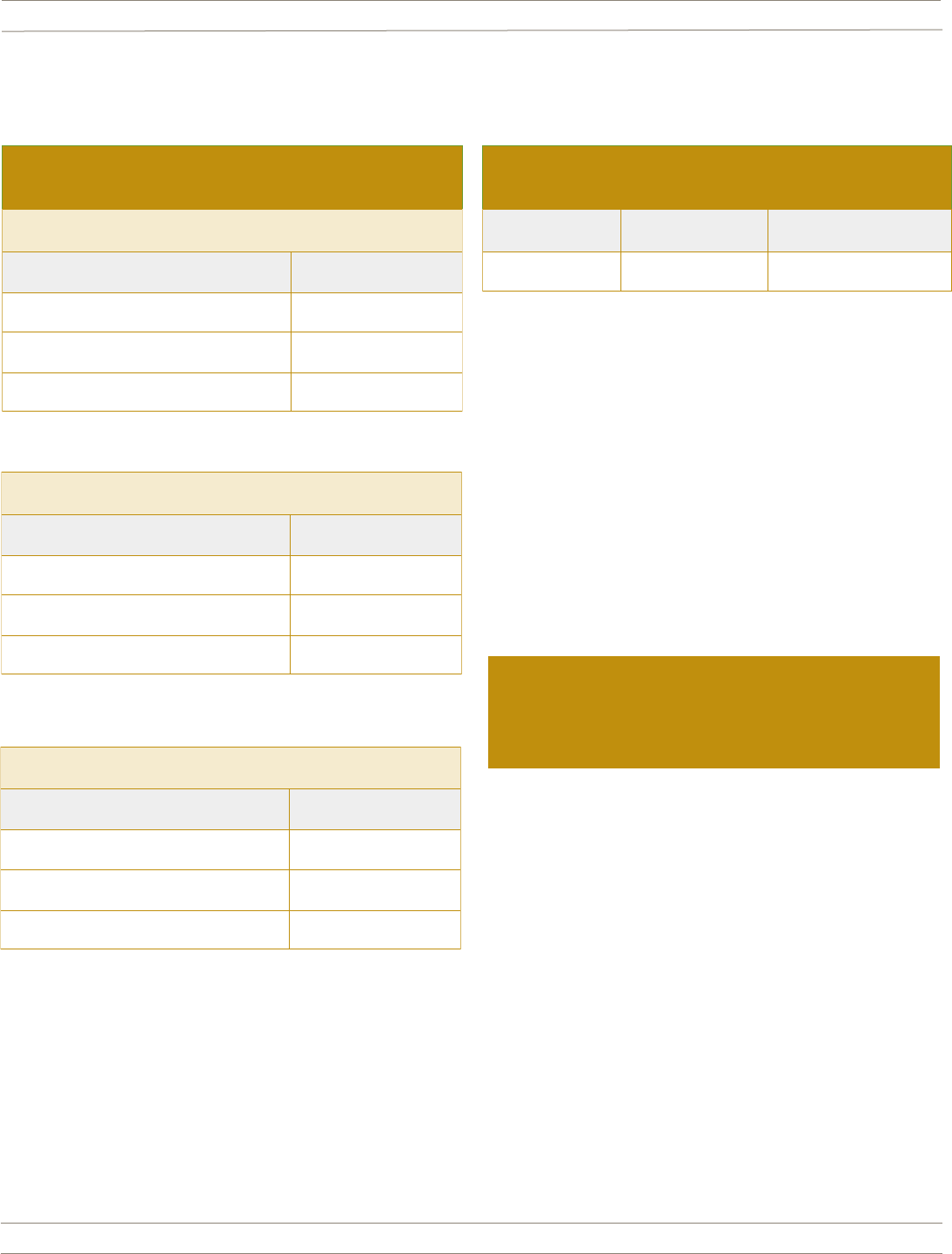
Member Prescription Cost Share
(no changes in 2023)
UP TO 30 DAY SUPPLY AT RETAIL WALGREENS ONLY
CATEGORY YOU PAY
TIER 1: GENERIC $10.00
TIER 2: PREFERRED BRAND $35.00
TIER 3: NON-PREFERRED BRAND $60.00
UP TO 90 DAY EXTENDED RETAIL WALGREENS ONLY
CATEGORY YOU PAY
TIER 1: GENERIC $25.00
TIER 2: PREFERRED BRAND $87.50
TIER 3: NON-PREFERRED BRAND $150.00
UP TO 90 DAY EXTENDED RETAIL AMAZON PHARMACY
CATEGORY YOU PAY
TIER 1: GENERIC $20.00
TIER 2: PREFERRED BRAND $70.00
TIER 3: NON-PREFERRED BRAND $120.00
Member Prescription Cost Share for Specialty Drugs
(Up to 30 day supply only)
Specialty Generic Specialty Preferred Specialty Non-Preferred
$25 $50 $100
Self-Administered Specialty Drugs on SaveOnSP list:
Enroll in the Manufacturer Assistance Program and
you will pay $0.
Florida Blue 800.507.9820 or visit www.floridablue.com

Pasco County Schools: Pharmacy Benefit
46
Member FAQs - Pharmacy
Q: I currently have prescriptions filled through Express Scripts
Home Delivery. Do they automatically transfer to the new
Amazon Pharmacy?
A: Yes, the medications will move over to Amazon Pharmacy if
your prescription has refills and is not expired.
Q: What happens if I do not have any refills left or my
prescription has expired?
A: If your prescription expires before January 1, 2023 or you will
have no refills on January 1, 2023, contact your doctor. Please
ask them to send a new prescription to Amazon Pharmacy on or
after January 1, 2023.
Q: What is the contact information for Amazon Pharmacy?
A: For questions, call Amazon Pharmacy Customer Care at
855-965-7539, Monday through Friday, 8:00 a.m. – 10:00 p.m.
ET and Saturday and Sunday, 10:00 a.m. – 8:00 p.m. ET.
Q: How do I transfer my refills to Walgreens Pharmacy?
A: Call or stop by your local Walgreens and tell the pharmacist you
want to move your prescriptions from another pharmacy. They’ll
help you make the switch. Just have a list of your current
medications handy.
OR
Using the free Walgreens mobile app on your smartphone, take
a picture of your medicine bottle and send it to your nearest
Walgreens.
Q: If I have an existing authorization on file for one of my
medications, will I need to get a new one?
A: No, as long as the authorization on file is still valid and has not
expired, Walgreens should be able to run the script and the
claim should pay. Some exceptions may apply. For example,
if the medication is refilled too soon, it may deny.
Q: Are there certain classes of medications that DO NOT transfer
and require a new prescription from your prescriber?
A: Yes, the following classes of medications would require a new
prescription from your prescriber.
• Narcotics for pain
• Medications to treat ADHD and other behavioral health conditions.
Q: What happens if I use another retail pharmacy other than
Walgreens?
A: For HMO Members, your medications will NOT be covered. You
will have to pay the full price of your medication out of your pocket.
For PPO Members, you’ll pay the full price of your medication and
can file a claim for reimbursement.
Your reimbursement will be
based on out-of-network benefi
ts.
Florida Blue 800.507.9820 or visit www.floridablue.com
1
Not all medications can be filled online.
Accredo is a specialty pharmacy that is contracted to provide services to members of Florida Blue. Accredo is a trademark of Express Scripts Strategic
Development, Inc.
Florida Blue is an Independent Licensee of the Blue Cross and Blue Shield Association.
We comply with applicable Federal civil rights laws and do not discriminate on the basis of race, color, national origin, age, disability or sex.
ATENCIÓN: Si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 1-800-352-2583 (TTY: 1-877-955-8773).
ATANSYON: Si w pale Kreyòl Ayisyen, gen sèvis èd pou lang ki disponib gratis pou ou. Rele 1-800-352-2583 (TTY: 1-800-955-8770).
107916 1021
Specialty drugs can be expensive. That's why as part of Florida
Blue’s SaveOn Program, Accredo Specialty Pharmacy will be your
exclusive provider for most of your specialty medication needs.
They help members like you save money on specialty drugs. Some
drugs may even qualify for a $0 cost share after copay assistance is
applied. You can call the number on the back of your Florida Blue
ID card to verify if your medication can be filled by Accredo.
Working with Accredo is easy!
• Refill prescriptions online at accredo.com or by phone at
888-425-5970
1
• Have medicine shipped to your home so you’ll have it
when you need it
• Receive around-the-clock, personalized support from a
specialty-trained pharmacist, even on holidays
Members must use Accredo for all specialty
prescriptions.
When drugs don’t qualify for $0 cost share, Accredo works with
you to find financial support to help with the cost. Please note:
Manufacturer coupons do not apply toward your yearly
deductible or out-of-pocket maximum. If you’re not eligible
for financial help or you choose not to receive it, you’ll be
responsible for your standard specialty copay. Any medications
not able to be filled by Accredo can be filled through the
specific designated pharmacies. Please check your medication
guide for a current listing of those pharmacies.
Save Money
on Specialty Drugs
Call Accredo now
to get started!
Call 888-425-5970, and a
pharmacy representative will
walk you through the process.
Be sure to have your Florida Blue
member ID, doctor’s name and
phone number, and your current
pharmacy and prescription
information ready.
We’re here to help.
If you have questions about your benefits or using Accredo,
please call the number on the back of your member ID card and
we’ll be happy to help.
Pasco County Schools: Pharmacy Benefit
48
Specialty drugs can be expensive. That’s why your pharmacy plan
with Pasco County School Board will include the SaveOn Program.
To participate, Accredo Specialty Pharmacy will be your exclusive
provider for most of your self-administered specialty medication
needs. They help members like you save money on specialty drugs.
Some specialty drugs may qualify for a $0 cost share after copay
assistance is applied.
Below are some member FAQ’s regarding the SaveOnSP Program.
2023 SaveOnSP Program Member FAQ’s
QUESTIONS ANSWER
Which specialty medications are impacted?
• Only self-administered specialty medications filled under your
pharmacy benefit are impacted.
• Physician administered medications, which are covered through
your medical benefits under medical pharmacy, will NOT be impacted.
Will a member using a specialty pharmacy
other than Accredo have to move their specialty
medications to Accredo?
• Yes, if the specialty medication is not a Limited Distribution Drug (LDD)
then the member has to switch to Accredo.
• If the specialty medication is a Limited Distribution Drug (LDD) and
Accredo is listed as a specialty pharmacy, then the member has to
switch to Accredo. See link below to the list of LDDs.
• http://www.bcbsfl.com/DocumentLibrary/Providers/Content/Rx_
LimitedDistributionDrugs.pdf
I received a call to enroll on the SaveOn Program.
Is this a scam?
• No, this is not a scam. You will save money by enrolling in the SaveOn
Program. If you do not enroll you may have to pay 30% or more
coinsurance for your self-administered specialty drug.
How to I find out if my specialty medication is part
of the SaveOn Program?
• Please contact Patty Nguyen, Florida Blue On-site Representative at
813-794-2492 or email her at Patricia.Nguyen@bcbsfl.com to inquire
if your specialty medication is part of the SaveOn Program.
What will the member’s cost share be for their
specialty medications under the SaveOn Program?
• $0 cost share if your medication is on the SaveOn list and you qualify
for and participate in the manufacturer assistance program.
• If you are taking a specialty medication that does not qualify for the
manufacturer assistance program, then you will pay the following cost
shares for specialty medications: $25 copay/$50 copay/$100 copay
(up to 30 day supply only)
How long will a member receive the $0 cost share if
his/her medication is part of the SaveOn Program?
12 months
What number do I call to reach Accredo regarding
the SaveOn Program?
1-888-425-5970
Florida Blue 800.507.9820 or visit www.floridablue.com
Pasco County Schools: Pharmacy Benefit
49
2023 SaveOnSP Program Member FAQ’s
QUESTIONS
ANSWER
Do members have to sign up for the manufacturer
assistance programs every year?
• Members do have to recertify for the manufacturer assistance programs
annually or at the manufacturer specified times.
• Accredo can assist members with understanding when they need to
recertify when they call in to schedule their next refill.
Will Accredo assist the members with applying for
the manufacturer assistance programs?
• Yes, the team at Accredo will assist the members with applying for and
getting approved for the manufacturer assistance program.
• For the manufacturer assistance programs that do not allow the team
at Accredo to assist, the team will provide the member with all the
information they require.
What happens if a member’s provider prescribes a
new medication that is part of the SaveOn program?
Can multiple members on the same contract be
enrolled in this program?
• Accredo will assist the member with getting set up on the manufacturer
assistance program for the new medication.
• Yes, this program is driven by the medication, not the contract.
• Multiple members within the contract can be on the program and
members can have multiple medications on the program as applicable.
Will manufacturer assistance program /coupons
count towards the member’s calendar year out of
pocket maximum and calendar year deductible?
• No, these amounts will not count towards the member’s calendar year
out of pocket maximum or calendar year deductible. The member will
have a $0 cost share for any specialty medication that qualifies under
the program.
Florida Blue 800.507.9820 or visit www.floridablue.com
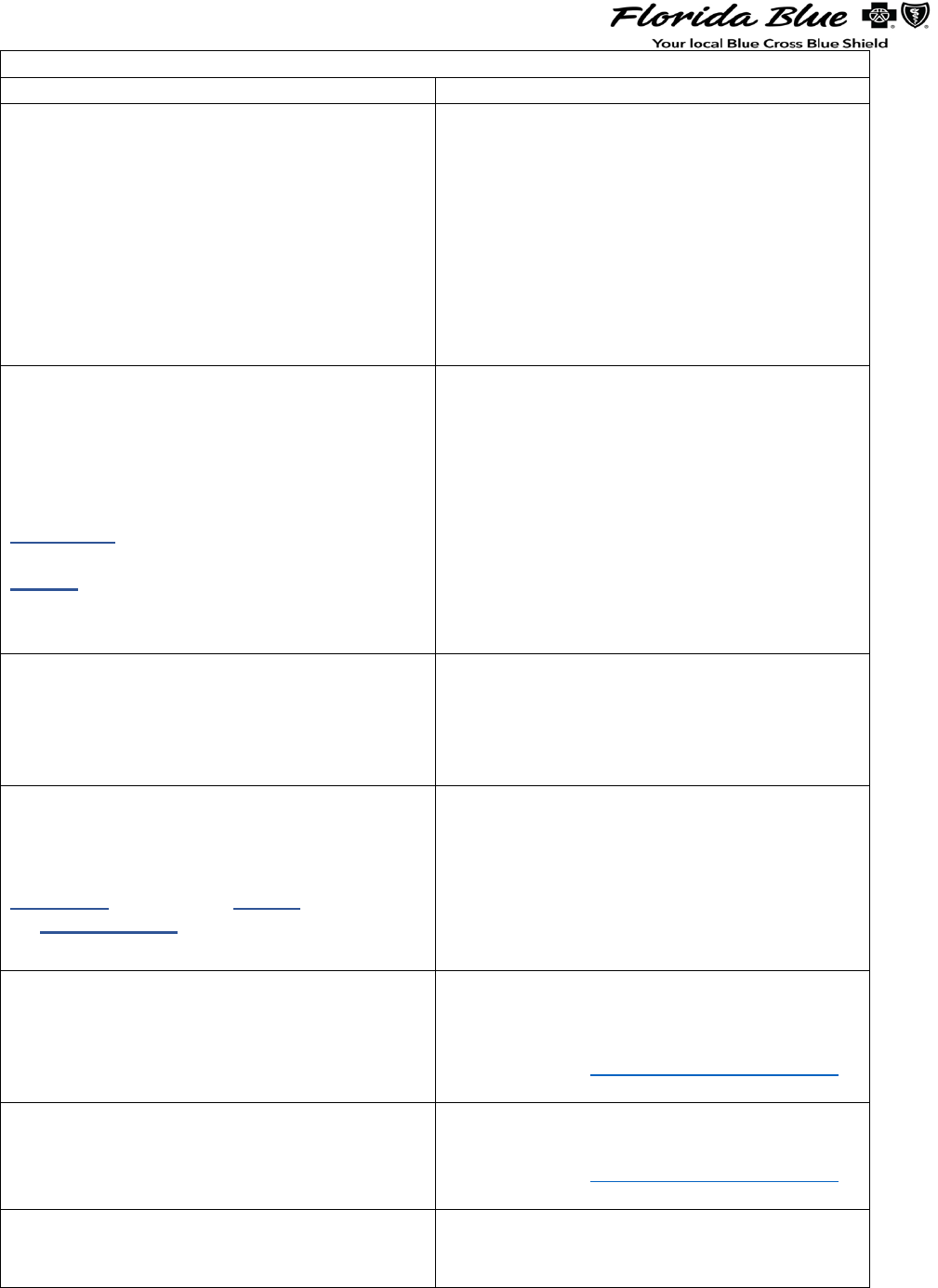
2023 PHARMACY OPTIONS
PHARMACY NAME
TYPE(S) OF MEDICATION
Walgreens Retail Pharmacy Exclusive
*Up to 30 to 90 days supply
• Only retail pharmacy you may use
to fill generic and/or brand name
medications (NOT self-
administered specialty
medications, provider-
administered specialty
medications or mail order.)
• Diabetic Testing Supplies (test
strips, lancets, glucometers, etc.)
• Insulin, Antibiotics
Accredo Specialty Pharmacy
1-888-425-5970
*Up to 30 days supply only
Exception: If your specialty medication is
a Limited Distributed Drug (LDD) and
cannot be supplied by Accredo, then you
may be able to use another specialty
pharmacy.
• Self-Administered Specialty
Medications. These medications
require Prior Authorization.
• Certain specialty medications may
be eligible for $0 member cost
share through a Manufacturer
Copay Assistance Program with
the SaveOn Program.
• Enrollment in the SaveOn Program
required. Contact Accredo for
assistance.
NEW Amazon Pharmacy Home
Delivery MedsYourWay
1-855-206-3605 (Prescribers only)
1-512-884-5981 (Fax #)
*Up to 90 days supply
• Long-Term Medications, i.e.,
blood pressure, cholesterol
medications, etc.
• For questions on setting up an
account, call
1-855-965-7539.
CVS CareMark Specialty Only
1-866-278-5108
Exception: Medication cannot be supplied
by CVS Specialty or Physician
participating in Buy & Bill Program.
• Specialty Medications
administered in a doctor’s
office/facility.
• Prior Authorization may be
required.
• Claims are submitted under the
medical benefit, NOT pharmacy.
My Health Onsite (MHO)*
1-888-644-1448
*Registered Patients
• Ask about select generic and
brand name medications at low
or no cost to you.
• Access www.pascogohealthy.net
for a list of covered medications
Elect Rx (District Program Offering)
1-844-353-2879
*Up to 90 days supply
• Select brand name medications
at low cost.
• Access www.pascogohealthy.net
for a list of covered medications
TrueNorth Meds Insulin Program
(District Program Offering)
1-844-681-8783
• Brand Name Insulin at low cost
